Promising new treatment for recurrent pediatric brain cancer
Two pediatric brain cancers that are challenging to treat if they recur, medulloblastoma and ependymoma, are the target of a clinical trial using a new type of therapy. A multi-institutional, international team led by researchers at ˛ÝÁńÉçÇřČëżÚ, Texas Children’s Hospital and the Hospital for Sick Children (SickKids) has developed a novel approach that delivers appropriately-targeted chimeric antigen receptor (CAR) T cell therapy directly into the cerebrospinal fluid that surrounds the tumor.
The researchers report in the journal that this approach was effective in treating these cancers in mouse models of human disease. The findings support further clinical studies to evaluate this strategy to treat pediatric brain cancers, the most common cause of cancer death in childhood. Indeed, a first-in-child clinical trial currently is recruiting patients at Texas Children’s Hospital and ˛ÝÁńÉçÇřČëżÚ to the safety and anti-tumor efficacy of this approach.
“Recurrences of medulloblastoma and ependymoma can be disseminated throughout the lining of the brain and spinal cord, which are bathed in cerebrospinal fluid. This location offers the opportunity to deliver therapies into the cerebrospinal fluid compartment and could provide a better chance for the therapy to reach and eliminate the tumor than administering it through the blood stream,” said co-corresponding author Dr. Nabil Ahmed, associate professor of pediatrics and immunology, section of hematology-oncology at Baylor and Texas Children’s Hospital.
“The vast majority of children with recurrent metastatic medulloblastoma or ependymoma currently have a deadly prognosis, so it is very exciting to think we have identified a novel approach to treat this underserved patient population,” said co-corresponding author , neurosurgeon, senior scientist in the Developmental and Stem Cell Biology program, Garron Family Chair in Cancer Research at SickKids, and professor in the Departments of Surgery and Laboratory Medicine and Pathobiology at the University of Toronto.
This project was led by Dr. Laura Donovan, post-doctoral fellow in the Developmental and Stem Cell Biology program at SickKids, who performed in-depth molecular studies of the target profile of recurrent medulloblastoma and ependymoma to guide the design of CAR T cells engineered by Ahmed and colleagues at Baylor’s Center for Cell and Gene Therapy and Texas Children’s Hospital to target the most appropriate cancer molecules.
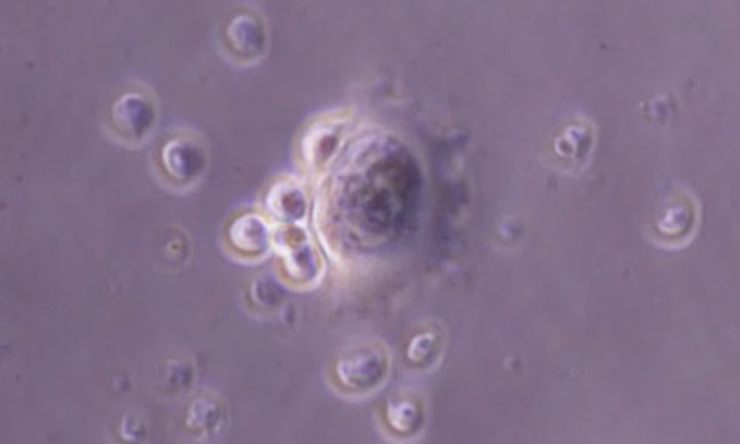
CAR T cells are a form of immunotherapy involving engineering of T cells, a type of immune cell that fights cancer. The researchers genetically engineered CAR T cells to recognize specific molecules on the surface of the tumor cells. When these CAR T cells encounter the tumor, they can fight it more effectively. CAR T cells have been impressively effective for patients with certain types of leukemia and are FDA-approved for this disease.
In mouse model studies, CAR T cells were administered into the cerebrospinal fluid around the tumor or into the blood stream of mice harboring multiple patient-derived medulloblastoma and ependymoma tumors. The tumor size and animal survival were studied for about 200 days.
The results showed that administering tumor-specific CAR T cells into the cerebrospinal fluid was more effective than administering them via the blood.
“As opposed to delivery through the blood, cerebrospinal fluid delivery overcomes the blood-brain barrier and also offers the advantage of minimizing exposure of other tissues of the body to the CAR T cells and, consequently, potential side effects,” Donovan said.
In some of their experiments, the researchers combined CAR T cells with an approved cancer medication called azacytidine. The results showed that combining immunotherapy with azacytidine was significantly more effective than either treatment alone.
“This work was possible thanks to the concerted collaboration of our Pediatric Cancer Dream Team supported by Stand Up To Cancer® (SU2C) St. Baldrick’s Foundation Translational Research Grant, which brought together scientists studying tumor genomics and tumor immunotherapy around the world to enable the design of more effective therapies for children with incurable and hard to treat cancers,” Ahmed said.
of all the contributors, their affiliations and financial support for this project.



 Credit
Credit