Q1: Which of the following morphological features most strongly suggest a metastatic tumor rather than a primary tumor origin?
A) Adenocarcinoma without any overlying precursor lesion
B) Extensive lymphovascular invasion in lamina propria or superficial
submucosa
C) Endoscopic and radiological correlation
D) All of the above
Answer: D. All of the above.
Explanation for Q1:
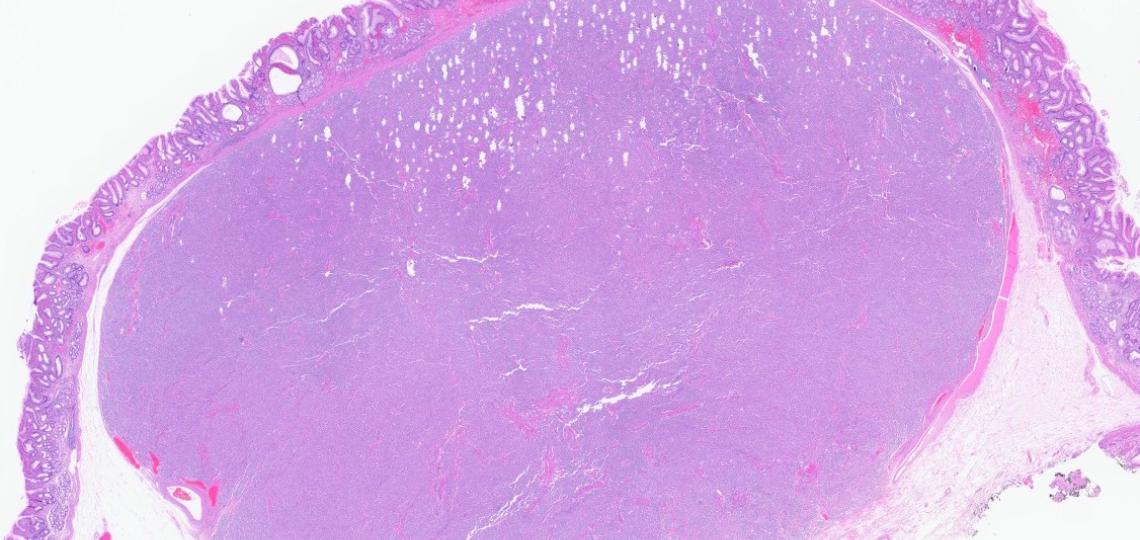
The biopsy of the rectal mass demonstrated infiltrating irregular glands within the submucosa. Importantly, the overlying epithelium was unremarkable, showing no evidence of dysplasia (refer to the PowerPoint image).
While metastatic adenocarcinoma to the rectum may occasionally involve the surface epithelium through cancerization, this case lacked any precursor lesions such as tubular adenoma or high-grade dysplastic changes.
The presence of extensive lymphovascular invasion in the lamina propria and superficial submucosa supports a metastatic origin rather than a primary rectal neoplasm. Correlation with endoscopic findings and imaging studies is crucial before finalizing the diagnosis.
Histologically, the tumor exhibits glands lined by cuboidal cells with a low nuclear-to-cytoplasmic ratio, basally located round nucleus with mild pleomorphism, and infrequent mitoses unlike primary colorectal adenocarcinoma, which usually shows columnar epithelium with stratified oval nuclei, frequent mitosis/apoptosis or dirty necrosis, further supporting the likelihood of a metastatic process.
Although metastatic carcinoma in the rectum is uncommon, differentiating between primary and metastatic cancer can be particularly challenging, especially when biopsies are conducted by a gastroenterologist.
As per the literature, potential sources of metastasis include pancreaticobiliary adenocarcinoma (as in this case); endometrial carcinoma, ductal carcinoma of the breast, ovarian serous carcinoma (in females); prostatic adenocarcinoma (in males), and others such as bladder, gastric carcinoma, and melanoma.
Metastasis of pancreaticobiliary carcinoma to the rectum is exceptionally uncommon but can occur. Therefore, heightened clinical suspicion, thorough diagnostic workup, and close follow-up are essential.
Pancreaticobiliary carcinomas are among the most aggressive malignancies, often carrying a poorer prognosis than primary intestinal tumors. When rectal metastasis occurs, it may mimic primary rectal cancer, complicating both diagnosis and management.
Q2: Which of the following immunoprofile will support diagnosis of metastatic adenocarcinoma of pancreatobiliary origin over intestinal/colorectal type primary tumor?
A) CK7 patchy positive, CK20 diffuse positive, CDX2 strong positive,
MUC1 Negative, MUC 2 positive
B) CK7 diffuse positive, CK20 patchy positive, CDX2 weak positive,
MUC 1 positive, MUC 2 Negative
C) CK7 negative, CK20 diffuse positive, CDX2 weak positive,
MUC 1 negative, MUC 2 positive
D) CK7 patchy positive, CK20 patchy positive, CDX2 weak positive,
MUC 1 negative, MUC 2 positive
Answer: B. CK7 diffuse positive, CK20 patchy positive, CDX2 weak positive, MUC 1 positive, MUC 2 Negative
Explanation for Q2:
Accurate identification of the primary site of a metastatic adenocarcinoma is essential for appropriate treatment planning and patient management. The expression patterns of CK7 and CK20 vary depending on the tissue of origin, making them valuable markers in determining the source of metastatic disease.
Immunohistochemical profiling using CK7, CK20, and CDX2 offers critical diagnostic information in pinpointing the primary site. Additionally, mucin stains such as MUC1 and MUC2 further aid in differentiating between primary tumor origins, enhancing diagnostic accuracy.
The pancreaticobiliary-type adenocarcinomas are more aggressive compared to the intestinal type. Since morphologic distinction can be challenging, immunohistochemistry has been advocated to make this distinction as the histologic subtype (intestinal vs pancreaticobiliary) can help in the choice of adjuvant therapy.
| Tumor Type | Positive Markers | Negative/Weak Positive Markers |
|---|
| Intestinal type | CK20 or CDX2 or MUC2
CK20, CDX2, and MUC2 (irrespective of MUC1) | MUC1 |
| Pancreatobiliary-type | MUC1 | CDX2 and MUC2 (irrespective of CK20) |
References
Olivier Janjic et al.Metastasis to the rectum: A systematic review of the literature,European Journal of Surgical Oncology,Volume 48, Issue 4,2022, Pages 822-833, .
Galanopoulos M, Gkeros F, Liatsos C, Pontas C, Papaefthymiou A, Viazis N, Mantzaris GJ, Tsoukalas N. Secondary metastatic lesions to colon and rectum. Ann Gastroenterol. 2018 May-Jun;31(3):282-287. doi: 10.20524/aog.2018.0244. Epub 2018 Mar 3. PMID: 29720853; PMCID: PMC5924850.
Sanjay Kakar, MD*; Chanjuan Shi, MD, PhD*; N. Volkan Adsay, MD; Patrick Fitzgibbons, MD; Mary K. Washington, MD, PhD: CAP Cancer and CAP Pathology Electronic Reporting Committees. Protocol for the Examination of Specimens from Patients with Carcinoma of the Ampulla of Vater
Tianzhu, Q., Xiaohan, W., Yang, L., Wen, P., Yirui, Z., Rui, Yanhong, G. (2022). Pancreatic metastases to the rectum: a case report and literature review. All Life, 15(1), 1325–1329. .
Digestive System Tumours, WHO Classification of Tumours, 5th Edition, Volume 1, WHO Classification of Tumors Editorial Board, 2019, ISBN-13.
Brian O’Sullivan, Thomas Burton, Ralph Van Dalen, Fraser Welsh, Archana Pandita, Jesse Fischer, Beware the pancreatic incidentaloma in colorectal tumours: pancreatic adenocarcinoma with metastases to the colon and rectum, Journal of Surgical Case Reports, Volume 2022, Issue 1, January 2022, rjab629,
Pernick N. MUC2-MUC6. PathologyOutlines.com website. . Accessed April 17th, 2025.